If you’ve ever had one of those winter seasons when you seem to pick up cold after cold, you’ll know that the experiences of each instance can be quite different even if there are some common symptoms.
Depression is a little like the common cold in that it’s an umbrella term that describes a collective of various types of dysfunction – Depression also comes in different shapes & sizes.
Here are a few of the more common types:
Unipolar Depression – The sufferer experiences a severe depression without experiencing relief or highs.
Bipolar Depression – Formerly known as Manic Depression, it is characterised by extreme highs & lows. The individual sufferers mood swings between the two extremes over time periods, either rapidly over short periods or slowly over longer periods of time. This particular form of depression requires professional support & treatment will usually involve medication to stabilise the sufferers swinging moods in addition to anti-depressants and supported with counselling & psychotherapy, ideally coordinated by a mental health team.
Major Depression – Formerly known as Chronic Depression, typically suffers are apathetic, experience persistent low mood, and are disinterested in activities. The symptoms must persist for at least 2 weeks for a diagnosis.
Mild Depression – The sufferer finds engagement with daily functioning & activities difficult and has a sense of living an unfulfilled life. This type of depression is usually exogenous in nature, i.e. is triggered and influenced by life circumstances & environmental factors.
Atypical Depression – There are parallels with the symptoms of Major Depression however, the sufferer may experience periods of happiness & enjoyment along with fatigue, and excessive sleeping & eating. The sufferer has a tendency to feel that their depression is influenced by external events & life circumstances. This form of depression can last for very long periods of time, potentially life-long.
Persistent Depressive Disorder – Formerly known as Dysthymia, the symptoms of depression include an inability to find enjoyment in life, dissatisfaction with life, feeling unimportant, often scared but do not recognise their symptoms as an illness – Moreover, seen as an integral part of life. The experience may include periods of Major Depression.
Psychotic Depression – Sufferers experience frightening or negative hallucinations.
Seasonal Affective Disorder – Also known by its acronym SAD, it includes mood swings that seem to be influenced by the seasonal cycle, often with the worst of symptoms experienced during the winter months.
Postnatal Depression – Often erroneously called The Baby Blues, it is a condition which may develop, usually between weeks 4 & 6 following giving birth although it can begin before or after that period. Symptoms can include mood swings, lack of interest in both oneself and/or the baby, low energy & fatigue, and decreased libido.
Premenstrual Dysphoric Disorder – Symptoms are usually strongest in the final week of menses but improving following the onset of menses.
As discussed in our previous post, the term depression is now commonly used to describe a range of human experiences, and all too often, not for depression in the forma; sense. This has many unfortunate consequences, one such example being that the experiences of sufferers is often reduced to the impression that depression is little more than feeling sad or being lazy and can be remedied simply by cheering up & pulling yourself together.
Such ideas completely fail to recognise the life changing illness that depression is; The cold war that goes on within ones own mind, and the potentially life threatening illness that it can become. I can’t stress this enough. Suicide is the most common reason for death in some cohorts of society – Young men being one such group, among whom suicide is about 3 times higher than in women of similar ages.
That is unlikely to change if the judgemental & misinformed common beliefs are lay-persons guide to treat sufferers with.
Treatment of Depression:
If the above sounds familiar and you think you may be suffering with depression I would urge you to step back from self-diagnosis and seek professional advice, starting with your GP. They will make an initial assessment & diagnosis and identify an initial treatment plan which will probably include prescribing some anti-depressants. However, there are some things that you can do which often help in treating & recovering from depression.
- Support Network: Consider your support network. Who are the main supports in your life that you can count on. Here are a few tips to help you identify a high quality support network:
- Professional Supports. These may include people like your GP, Psychiatrist, or a Counsellor & Psychotherapist, or any support groups that you may be attending.
- Informal Supports. These will include family & friends.
- Employer. Consider discussing your mental health with your employer. Not only will this give them the chance to make any necessary adaptions to your workload & work type but some employers have Employee Assistance Programmes which can provide access to funded counselling services.
Don’t simply list these out. Include information like hours of availability and details of the specific skills or qualities each can offer. After any engagements with each of these, go back & review your network and grade any particular person or agency you’ve contacted. The idea is to refine your network so in future you can contact the best option for you in any circumstance and at any particular time.
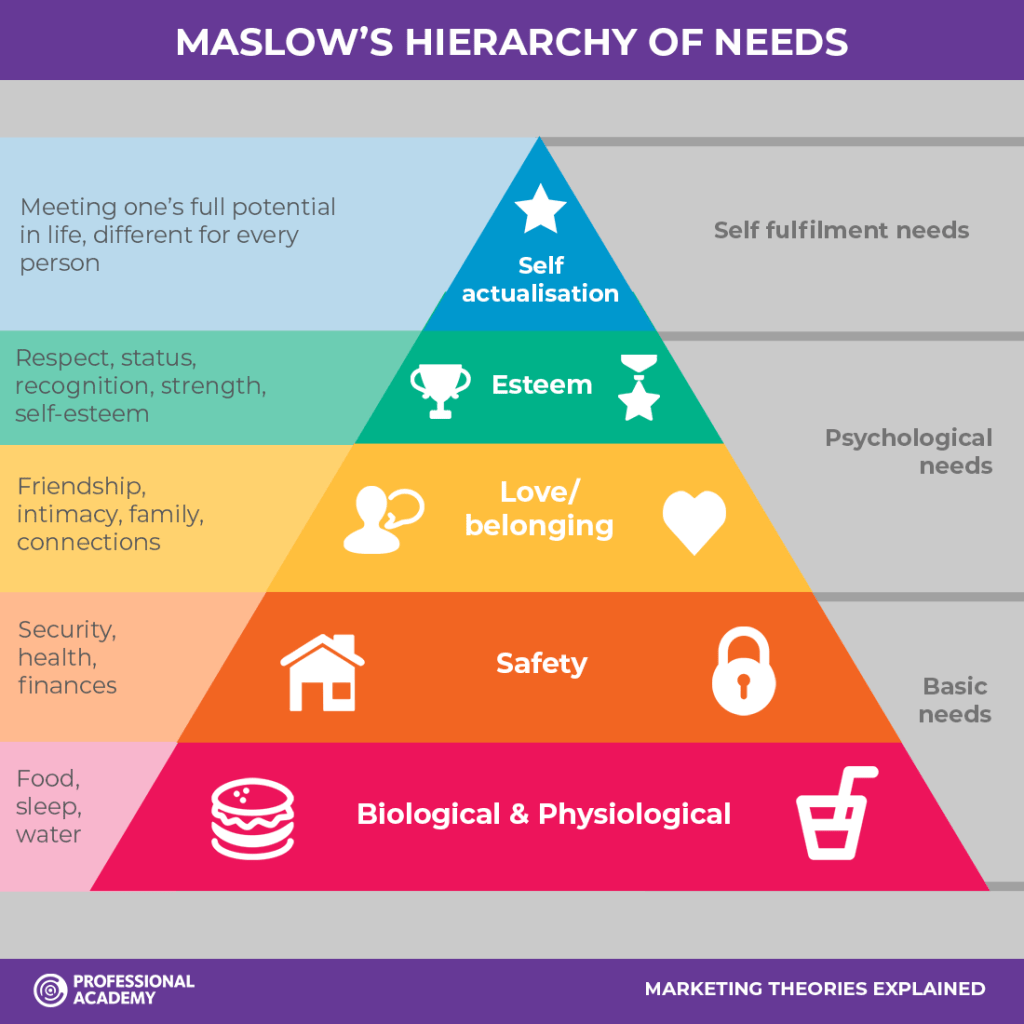
- What are your needs? Although Maslow’s hierarchy is not without it’s critics, it does offer a good model to assess how our intrinsic needs are being met. For example, does your diet provide sufficient quantity & quality for your needs, are you safe. These might sound like basic things that many of us take for granted in life but to many they produce a picture of the life circumstances that we find ourselves and help to breakdown the problem into its components that we can then begin to try to resolve.
- Exercise. This may well prompt some of you to dismissively sigh and wistfully think If only! But, research shows that exercise can be of real benefit in combatting depression and that effect is boosted further if you can get out in a natural setting like a woodland walk or park. However, I recognise that people who suffer with depression sometimes find it a major challenge just to get out of bed or complete daily tasks. The objective here isn’t to make anyone feel guilty about their level of ability. This something that you can do if health permits it. Speaking as a sufferer myself, I find the 2 minute technique useful – I privately commit to trying something like exercise for 2 minutes. If, at the end of those 2 minutes I still feel lousy, I decide whether to stop or carry on. I find that once I’ve actually started, I can usually keep going. In short, do what you can.
- Develop a self-care plan. It’s easy to fall into the trap of neglecting your personal hygiene & care. It’s often not a conscious choice. Often, depressed people feel too fatigued, lack the energy or simply don’t feel worthy of care. So, develop a self-care plan that identifies all the things you do to take care of yourself that help you feel better. It could be anything from taking a bath to getting a hair cut. We’re looking for any non-destructive self-care behaviour helps.
- Develop a coping plan. This is where you get creative. Identify things you do in life that give you a lift. Whether that’s watching your favourite TV show, listening to certain music, the company of a good friend. Whatever it is that helps you feel better. However, try to keep the plan to constructive habits and steer clear destructive behaviours like drinking, abusing substances or self-harming. If these are a part of your current coping strategy I advise seeking professional advice to help you grow away from these destructive practices & develop new coping strategies.
- Tailor your plan. Have a plan for the bad days & a plan for the better days.
If you would like to talk about depression please get in touch with us at BroadMinds Therapy for a private & confidential conversation. You can reach us using any of the following contact details:
Phone: (+353) 0899420568
Email: hlpe@broadmindstherapy.org
Web: http://www.broadmindstherapy.org
Facebook:
