Self-Harm: “It’s just a cry for attention!”
Suicide: “So selfish. What a coward!”
How often have you heard these statements or something like them?
Continuing our theme for May on The Legacy of Lockdown, we’re looking at another issue that long predated the Coronavirus pandemic. The impact of the pandemic on mental health has received regular attention in the press which has been something of a double-edged sword. While it helps to foster awareness and distribute information, the information is often misleading or false and can give governmental institutions the opportunity to pay lip service to the cause while doing very little to actually progress it.
The same is often true across the range of mental health issues but on this occasion I’m talking about self-harm & suicide.
Because of the way data is collected & analysed, the full effect of the pandemic on rates of self harm & suicide aren’t yet fully known and may never be.
In Ireland, there is some confusion about the veracity of the data available. In October 2020 the TD claimed that hospitals weren’t recording data at all, suggesting that data collection on self harm & suicide rates was suspended during the first period of lockdown until around July 2020. However, data is available which suggests that rates were on the whole, comparable to rates in 2018/19. As a caveat to that I should add that rates in February 2020 showed an increase of around 18% before dropping significantly in March & April in comparison with 2019.
However, the criteria for qualification as an instance to be recorded as a case of self harm is by the presentation of a self harm related injury or illness at a hospital. In other words, only those reporting at a hospital get recorded in official figures and even then, it’s hard to have faith in the figures when the TD says the data isn’t even being collected; But, even when the data collection system is in operation, all the cases of self harm that are never presented at a hospital slip right through the net.
In the UK figures are still being collected & analysed although early indications are that the suicide rate has largely been unaffected, disregarding the usual variances that often occur from time to time.
Globally, data broadly reflects the same trend – that suicide rates are consistent in comparison with previous years. However, some countries such as New Zealand, Australia & Japan have reported a fall in rates. I have no data to support a conclusion but the perception from this part of the world is that these three countries handled the pandemic really well – And I wonder how that influenced stress & anxiety levels among their peoples.
Research suggests that around 210 out of every 100,000 in Ireland and 400 people out of every 100,000 in the UK self-harm. It is worth noting here though, that numbers of people self-harming are likely much higher. These figures only represent those presenting at medical facilities for assistance with their injuries, where as the majority of self harm incidents aren’t likely reported at all.
The number of people self-harming is on the increase, rising by just over 16% since 2002 and the data suggests that those who self-harm are doing so more with instances rising by around 19% over the same period.
So what’s going on? What is driving more & more people to self-destructive behaviour?
People who self-harm do so in an attempt to cope with suffering & distress that they may find hard to articulate or cope with in other ways. It isn’t all about cutting yourself or harming in yourself in obvious ways. It can also be much more subtle. If you’ve ever reached for an alcoholic drink of some kind, smoked or taken some kind of drug to cope, you too have self-harmed. Clearly there are behaviours which are potentially more harmful than others but self-harm is as much about the motivation as it is about the specific behaviour.
Thoughts of suicide are surprisingly common and in some sectors of society, it is the leading cause of death. People don’t commit suicide because they are selfish or cowardly. Indeed, for many, they have lived with great courage in coping with life changing illnesses like depression for very long periods of time. It may start to feel like the only option for relief from their illnesses, even if there are other options. If we consider how someone with a life changing physical illness might prefer to be euthanised than live with the circumstances they find themselves in, we can begin to understand suicide a little more clearly.
There is no one answer to the question above as the following graphic illustrates. People of different ages and gender tend to self-harm in different ways & at different rates:
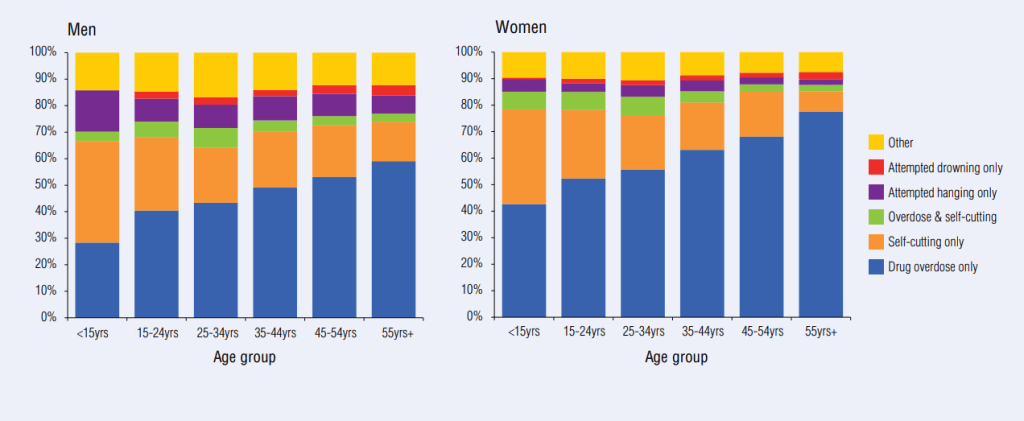
You can see from the charts above that cutting & over-dosing are the most common forms of self-harming across all ages & genders. However, the older you are the more likely over-dosing is to be your method of choice, while the younger you are, the more likely cutting is your method of choice.
This information is more than a point of interest. It can be used to guide us as when considering what we should look out for in each age & gender group. Of course, we need to be mindful of all types of self-harm when looking out for those we love but understanding what self-destructive behaviours people are more likely to turn to gives us a good starting point.
Also, if we consider the reasons why people turn to self-harming as a coping measure, we can take measures to prevent it from happening in the first place. What follows is a list of common reasons people self-harm:
- Work or school based stress
- Bullying or coercion
- Financial problems
- Being a victim of abuse, including physical, verbal & sexual
- Loss & Bereavement
- Confusion over sexuality
- Confusion over sexual identity
- Relationship dysfunction & loss
- Job loss
- Illness & poor health
- Low self-esteem
- Increases in stress levels
- Depression & anxiety
- Feelings of anger & numbness
People who self-harm often do so as a way of masking or displacing the emotional & psychological pain being experienced, for example, by any of the reasons above, with physical pain which they may find more manageable. In this way it is seen as a coping mechanism. Put simply, the self-harmer may be trying to replace one type of pain or distress with another kind that they find easier to cope with.
More common types of self-harm include:
- Overdosing – Including both prescription & non-prescription medications as well as illegal substances
- Substance misuse & abuse
- Cutting
- Burning
- Banging of the head or other body parts against hard objects
- Puncturing the skin
- Swallowing things
- Pulling out hair or eyelashes
- Self-tattooing
- Sadomasochistic practices
- Over-eating or under-eating
- Putting oneself in danger
Clearly this is not an exhaustive list but hopefully it informs & provides a snapshot of what to look out for; And apologies for the repetition from a previous post but this is so important I want to reinforce the kind of behaviours to look out for that might indicate that someone is self-harming – It’s simply too important not to know this:
- Becoming withdrawn.
- Unusual outbursts of frustration &/or anger.
- Changes in mood, particularly persistent low mood.
- Covering Up: Wearing clothes that don’t seem appropriate such as long sleeves on hot days, roll-neck sweaters, or changes in typical clothing choices that mask body parts that are usually visible.
- Signs of anxiety like constant fidgeting, twitching, pacing.
- Obvious signs of self-harm like picking & scratching at skin, pulling hair.
- Changes in eating & drinking habits.
- Changes in exercise levels.
- Accessing self-harming resources
- Peers:
- People are more likely to self-harm if their peers self-harm. Therefore, be mindful of the relationships that your friends & family maintain. If you think that a friend of theirs is self-harming or encouraging that behaviour, it may be time for careful intervention.
- Role Models:
- Again, people are more likely to self-harm if role models are known to self-harm, too, so be mindful of those they look up to.
My advice remains simple & straightforward: Don’t try to cope with this alone. Get professional help.
Preventing the Horror:
I like the idea that prevention is better than cure. Preventing mental distress that can result in mental illness begins before children are even born. People are often quick to accept that factors like diet & nutrition are important for pregnant mothers, but less so when considering their own childhood history. In short, the adverse childhood experiences of parents can have dramatic influences on the childhood of their children. My point being that addressing your own mental health can be a very important step if you want to make a good job of being a parent, yourself; And subsequently, your child’s ability to parent well. Parenting & child development is a topic for discussion another day, but to say that supporting parents to help them be the best they can at the most important job we have in society is surely something we should all aim for.
So how do we nurture the kind of mindset and good coping skills in our children that will serve them well as they face the tries & tribulations that life will inevitably present?
It has long been shown that children who develop healthy, secure attachment bonds with their parents are much less likely to suffer with mental distress in later life; Develop fulfilling intimate relationships with others, maintain & regulate their emotions, feel confident and good about themselves, enjoy the company of others, cope better with disappointment & loss, and are better at sharing feelings and seeking help when needed. You can find some great tips on helping to nurture such a bond on: https://www.helpguide.org/articles/parenting-family/building-a-secure-attachment-bond-with-your-baby.htm
Consider the common reasons why people self-harm, outlined above – Consider whether a friend or family member is experiencing any of these and think about how well they are coping with these issues & circumstances – What are their coping techniques & strategies and are they effective?
These are also common factors in other kinds of mental distress so when considering these, you may also uncover other areas of help that an individual needs.
Supporting the sufferer:
Of course, the very fact that self-harm is an increasing problem tells us that we also need interventions that help people who are already suffering. So what can we do to help?
- The first priority is to ensure your safety as a helper. Please don’t put yourself in harms way. If necessary call the emergency services.
- Assess the severity of any injury that the individual has. If you’re in any doubt about whether or not an injury needs medical attention, don’t think twice. Get medical help. Sometimes this can be difficult – The individual may not want medical attention. All you can do is your best in such an instance. If you think the injury is life threatening, don’t wait for them to agree.. Just call the emergency services regardless of the individual’s wishes. They may not be immediately thankful but hopefully they’ll come to understand your motivations.
- If the individual hasn’t yet injured themselves but you are concerned they might be suicidal, again, just call the emergency services & stay with them until help arrives if it’s safe for you to do so. Take the necessary measures to protect yourself – do not put yourself in harms way.
- Assuming that the sufferer is not in any immediate danger, the next step is to try to persuade them to seek out professional help. Often the first point of contact is the individual’s doctor. This can present opportunities for the assessment of any injuries, education on the dangers of the methods of self-harm being used, gain access to medicinal treatments as well as consider referrals to psychiatric or psychological support services.
- The list of items that can be used to harm ones-self is pretty much endless. If someone is determined to harm themselves they will find a way. However, you can remove access to any items that are usually used or any other dangerous items that could be used as an alternative. Objects like knives, lighters, needles, scissors are obvious things to look out for. Restrict access to any such items as much as you practically can.
- Get professional help. Needless to say that self-harming can be dangerous and the individual concerned will need help to tackle the cause of their problem, not just the self-harming, itself.
- Get non-professional help. Help the individual concerned identify & build a strong support network of friends & family that are available and have the right attitudes & qualities to help. It’s serves no one well having people in a support network if they make the individual feel worse or if they’re great at helping but are never available.
In summary, if you are supporting someone who self-harms, keep it simple. You don’t have to solve their problems for them.. Just listen without judgement & accept the individual concerned as they are. Get medical help if there are any immediate concerns but always seek professional help to address the ongoing problem.
If you recognise these signs in yourself or someone you know, it’s time to consider getting some professional help. Always remain aware of potential needs for medical assistance. If you or someone you know is suicidal then do not hesitate to contact the emergency services as soon as possible.
If you would like to talk about self-harm, whether it be for yourself or someone you know feel free to contact BroadMinds Therapy for help & advice. Call (+353) 0899420568, email help@broadmindstherapy.org , message us via this website, or visit our facebook page http://www.facebook,com/jpbroad for more information.
Finally, if you like what you read please like & share to help us reach & help as many people as possible.
Thanks for taking the time to read this article.
